Over 60% of Americans turning 65 this year underestimate their medical bills by $2,500 annually—even with federal health benefits. While eligibility often lowers spending compared to private plans, surprise fees and complex coverage rules create financial traps for unprepared retirees.
Part B premiums alone now average $185 monthly per person, with no family discounts. A couple could spend $6,000 yearly just for basic medical insurance. Add deductibles, prescriptions, and supplemental plans, and annual expenses exceed $7,000 per individual—a figure that shocks many new beneficiaries.
High earners face an added hurdle: IRMAA surcharges. These income-based adjustments can double premium costs, making early financial planning critical. Unlike disability insurance, which protects current income, post-retirement health strategies require balancing coverage gaps against long-term savings.
Key Takeaways
- Part A hospital coverage is usually premium-free for those with 10+ years of work history
- Medical insurance (Part B) costs $3,000+ annually per person, with no household rates
- Prescription drug plans (Part D) and supplemental policies increase total expenses
- Wealthier retirees may pay higher premiums through IRMAA adjustments
- Comprehensive budgeting should account for deductibles and unexpected care needs
Medicare Basics and Expense Overview
Three primary components form the foundation of federal health benefits for seniors. Each carries distinct pricing structures and enrollment rules that directly impact annual budgets. Timely enrollment and understanding coverage tiers can prevent thousands in penalties.
Breaking Down Hospital and Medical Coverage
Part A typically requires no monthly payments for those with 10+ years of work history. However, each hospital stay triggers a $1,676 deductible per benefit period. Extended care costs escalate sharply:
| Hospital Days | Daily Rate |
|---|---|
| 1-60 | $0 |
| 61-90 | $419 |
| 91-150 | $838 |
Part B charges $185 monthly even if unused, plus a $257 yearly deductible. Delaying enrollment adds 10% to premiums for each missed year—a permanent increase. “These penalties compound like credit card debt,” notes healthcare analyst Maria Torres.
Prescription Drug Plan Essentials
Part D premiums vary by location and medication needs. Most plans include deductibles and tiered pricing. Monthly rates jump 12% annually for late enrollment. For example:
- Blood thinners: $15-$45 copay
- Insulin: $35 monthly cap
- Specialty drugs: 25-33% coinsurance
Choosing pharmacies within plan networks often lowers out-of-pocket amounts. Review formularies annually—covered medications change more frequently than many realize.
In-depth Analysis of medicare costs retirement
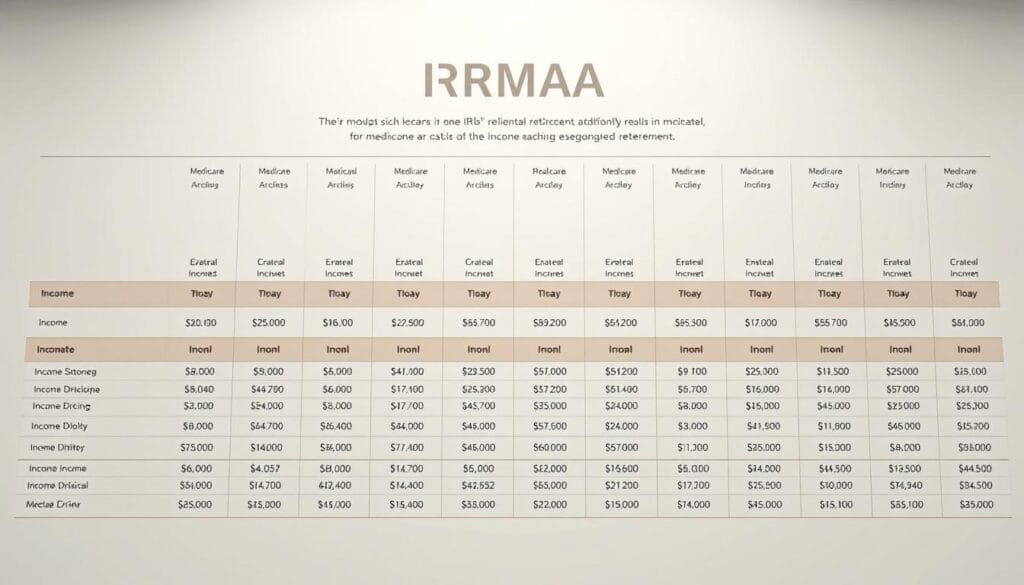
Many Americans face unexpected fee hikes due to a lesser-known rule tied to past earnings. The Income-Related Monthly Adjustment Amount (IRMAA) adds surcharges when modified adjusted gross income exceeds specific thresholds. These calculations use tax returns from two years prior, meaning today’s earnings could impact future premiums.
How MAGI Impacts Your Payments
Modified adjusted gross income includes wages, investments, and even tax-exempt bond interest. For 2025, a couple filing jointly with $220,000 MAGI from 2023 pays $259 monthly for Part B – 40% above standard rates. Part D adds $13.70 extra per month.
Common triggers include:
- Required minimum distributions after age 72
- Capital gains from home sales over $500,000
- Roth IRA conversions boosting taxable income
Case Studies: When Planning Matters
A Texas couple learned this firsthand after selling rental property. Their one-time $300,000 profit pushed Part B premiums up for two years. “We didn’t connect the dots between asset sales and health costs,” they admitted.
Another example involves municipal bond investors. Though interest stays tax-free, IRMAA counts it toward MAGI. This creates a 15-20% effective tax through premium increases. Strategic Social Security claiming strategies can help offset these surcharges when timed properly.
Annual income reviews become essential. A single $1,000 MAGI overage can cost $700+ yearly in extra fees. Work with financial planners to smooth out income spikes and avoid bracket creep.
Strategies for Reducing Healthcare Expenses in Retirement

Smart financial moves can significantly lower healthcare bills for older adults. Proactive planning helps avoid unnecessary surcharges while maximizing coverage benefits.
Tax Planning and Income Management Techniques
Timing major financial decisions is crucial. Selling property before age 63 or delaying pension withdrawals keeps income below IRMAA thresholds. Roth IRA conversions spread tax burdens across multiple years.
- Use Form SSA-44 to appeal surcharges after job loss or divorce
- Offset capital gains with tax-loss harvesting on underperforming stocks
- Direct charitable gifts from IRAs after 70½ to reduce taxable income
Utilizing Financial Advisors for Medicare Counseling
Specialized planners identify hidden savings opportunities. One client saved $1,200 annually by adjusting their retirement income strategies to avoid bracket jumps.
Advisors help:
- Coordinate Social Security claims with Roth conversions
- Analyze prescription drug plans during annual enrollment
- Create five-year income projections to smooth MAGI levels
Regular portfolio reviews prevent surprise fee hikes. As wealth manager Lisa Nguyen advises, “Treat healthcare budgets like investment portfolios—rebalance them yearly.”
Supplemental Coverage Options: Medicare Advantage and Medigap
Choosing the right supplemental coverage requires balancing immediate savings against long-term security. Two primary paths exist: bundled Medicare Advantage plans and standardized Medigap policies. Each offers distinct financial trade-offs for managing healthcare expenses.
Exploring the Benefits of Medicare Advantage Plans
These bundled options often feature $0 monthly premiums but require maintaining Part B payments. They cap annual out-of-pocket costs at roughly $5,000, after which plans cover 100% of services. Many include prescription drugs, dental care, and gym memberships.
Financial advisors recommend budgeting for double the maximum limit when evaluating these plans. “Back-to-back health events could drain $10,000 from savings if not planned for,” warns insurance expert David Klein. Network restrictions apply, so verify preferred providers participate before enrolling.
Medigap Cost Predictability vs. Flexibility
Standardized supplement policies offer premium predictability but higher upfront costs. A 65-year-old typically pays $150 monthly, with premiums rising about 10% yearly. These plans eliminate most copays and deductibles for Parts A and B services.
Key differences become clear when comparing options:
| Feature | Medicare Advantage | Medigap |
|---|---|---|
| Monthly Premium | $0+ | $150+ |
| Annual Maximum | $5,000 | None |
| Provider Network | Restricted | Any accepting Medicare |
As noted in this Medigap vs. Medicare Advantage comparison, supplement plans work best for those prioritizing provider choice. Both options require Part B premiums, making retirement savings plans crucial for covering base costs.
Planning for Future Cost Increases and Policy Adjustments
Financial forecasts for senior healthcare reveal annual premium hikes that outpace general inflation rates. While federal benefits provide foundational support, evolving policies and economic factors demand adaptable budgeting strategies.
Preparing for Premium Increases and Deductible Changes
Monthly payments for Part B and Part D typically rise 4-6% yearly. Medigap policies compound this pressure with 10% annual increases on average. A $150 monthly supplement today could cost $450+ in 15 years.
Three critical preparation steps:
- Review coverage annually during open enrollment
- Set aside 3-5% more yearly for health budgets
- Use HSAs or dedicated savings accounts for deductible spikes
Deductible structures change every October. Last year’s $226 Part B deductible jumped 8%—a trend likely to continue. “Plan for at least 5% growth in out-of-pocket maximums,” advises financial planner Rachel Kim.
Those with long-term care needs face compounded challenges. IRMAA adjustments and prescription formulary changes add layers of complexity. Multi-year projections help identify breaking points in coverage adequacy.
Key considerations for sustainable planning:
- Compare Advantage vs. Medigap every 3-5 years
- Track income thresholds to avoid surprise surcharges
- Balance immediate savings against lifetime cost ceilings
Conclusion
Effective planning transforms potential financial pitfalls into manageable healthcare expenses. While federal benefits reduce overall spending, gaps in dental, vision, and long-term care require separate strategies. Geographic factors also play a role—where you live affects supplement plan rates and access to services.
Work with specialists to navigate premium structures and income adjustments. Tools like estimating expenses help align coverage with budgets. Advisors can optimize Social Security timing and tax-efficient withdrawals to minimize surcharges.
Consider how income decisions impact monthly payments over decades. Regular reviews of policies and savings ensure your approach adapts to changing needs. Balance immediate savings with long-term security for lasting financial health.

